
[ad_1]
Selection process and research characteristics
From the initial pool of 463 articles identified for meta-analysis, 56 duplicates were removed, leaving 407 unique articles (Figure 1). These were pre-screened based on title and abstract, narrowing down to 28 articles selected for detailed full-text review. Rigorous evaluation of specific inclusion and exclusion criteria resulted in 11 articles being excluded for various reasons, resulting in a final set of 17 articles with a large participant pool of 6,642,297 participants. were deemed suitable and included in the meta-analysis.16,17,18,21,22,23,24,25,26,27,28,29,30,31,32,33,34.
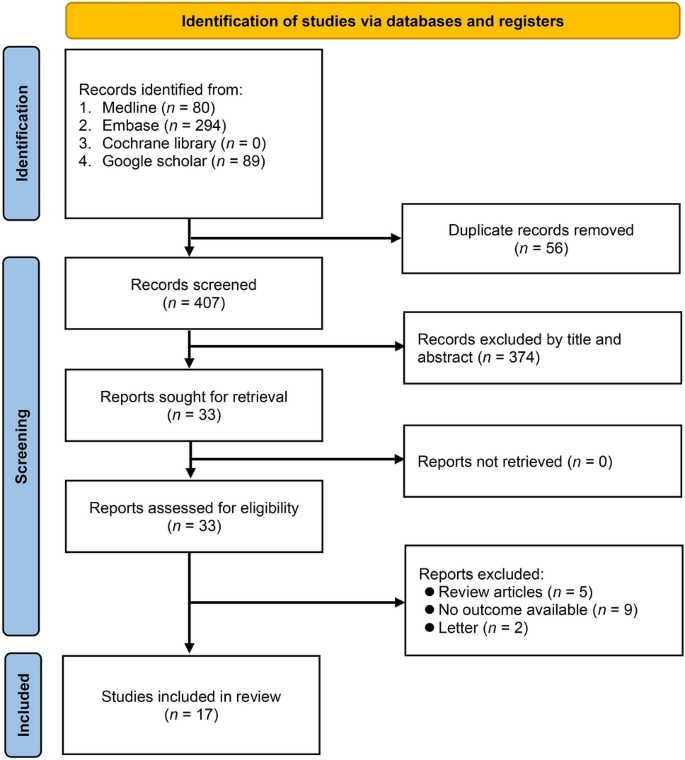
Selection of studies on the association between systemic sclerosis (SSc) and the risk of cerebrovascular and cardiovascular disease (CVD).
Table 1 summarizes the study characteristics. We thoroughly reviewed 17 studies across a variety of geographic regions, including Canada, Denmark, Taiwan, Belgium, Switzerland, the United States, and Copenhagen. These studies combined a wide range of participants; Kurmann et al.’s study included only 78 SSc patients.30 In the study by Thormann et al., the number reaches 8947.33. The average age of the participants in these studies varied, with Thormann et al.’s average age ranging from his 35 years of age.33. Up to 60.9 years in the study of Ying et al.16. A notable observation across these studies is the preponderance of female participants, with the proportion frequently exceeding 70%, e.g., reported as 91% in the study by Kurmann et al.30. Furthermore, the follow-up period varied between studies, with the shortest period of 1 year in the study by Thormann et al.33a study by Aviana Zubieta and colleagues lasted up to 14 years.twenty five.
quality of research
Table 1 summarizes the quality of studies using NOS. Approximately 53% (9 of 17) of the studies demonstrated high quality research methodology, as indicated by scores ranging from 8 to 9. On the other hand, approximately 41% (7 out of 17) of the studies were of moderate quality, with NOS scores of 6 to 7. A small portion of the studies, approximately 12% (2 out of 17), namely Hesselvig 2018 and Michel 2020.29,31This lower score could be due to potential limitations in participant selection, group comparability, or outcome measurement, thereby introducing a greater risk of bias.
Meta-analysis results
Main results
Of the 17 studies included in our meta-analysis, 11 reported data on the association between SSc and stroke risk.16,17,18,21,23,25,26,30,31,33,34. These studies included a total of 1,157,175 participants. The pooled HR for stroke in his SSc patients compared with the general population was 1.64 (95% CI, 1.35–2.01; p < 0.00001; I).2±82%) (Figure 2), suggesting a significant association between SSc and increased stroke risk. Subgroup analysis showed a significantly increased risk within the non-Asian subgroup (HR, 1.55; 95% CI, 1.26 to 1.9; p< 0.0001; I2≧77%). In contrast, individuals from the Asian subgroup (all from Taiwan)17,21,24,27,28,34 showed a trend toward increased stroke risk, but this trend was not statistically significant (HR, 1.86; 95% CI, 0.97 to 3.55; p = 0.06; I2≦=≦90%) (Figure 3).
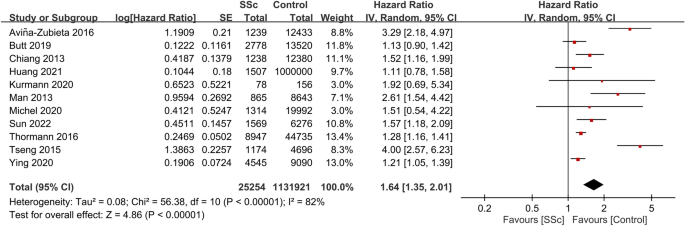
Forest plot showing the association between systemic sclerosis (SSc) and stroke risk. CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
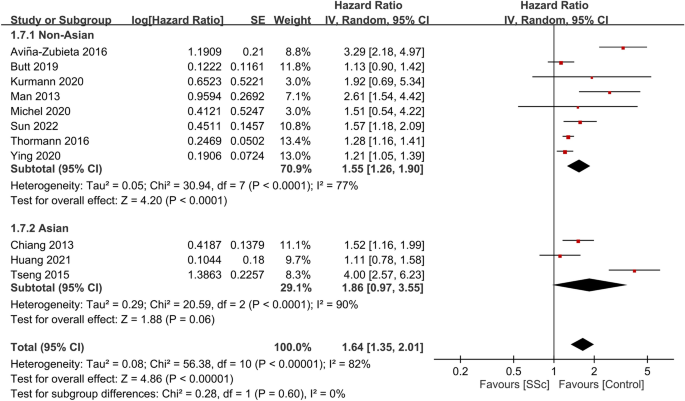
Subgroup analysis of stroke risk based on ethnicity (e.g., non-Asian vs. Asian). CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
To assess the stability of the results, subgroup analyzes were performed using only the largest cohort studies from each country. Therefore, the six studies16,21,23,25,31,33 For the primary outcome, the group with the largest sample size from different regions was analyzed. The overall HR for stroke in her SSc patients compared with the general population was found to be 1.46 (95% CI, 1.18–1.81; p = 0.0005; I).2≥78%) (Figure 4), showing consistent results.
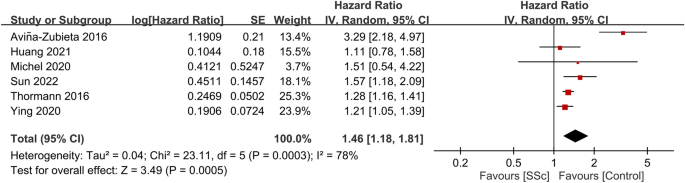
Subgroup analysis of stroke risk in systemic sclerosis (SSc) patients and the general population using the largest national cohort study. CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
secondary results
Seven studies provided data on CVD risk in patients with SSc. A total of 5,524,044 participants were involved, and the overall HR for CVD was 2.12 (95% CI, 1.36 to 3.3; p = 0.0009; I).2±98%)18,22,24,25,29,30,33. This suggests that SSc patients have a significantly increased risk of CVD compared to non-SSc patients (Figure 5). Consistently, data from seven studies including 116,023 participants showed a pooled HR of 2.15 (95% CI, 1.23 to 3.77; p = 0.008; I).296% of MI in SSc patients), indicating a significant association between SSc and increased MI risk (Figure 6).18,23,25,26,27,30,33. Additionally, SSc patients were observed to have increased her VTE risk (HR, 2.75; 95% CI, 1.77 to 4.28; p < 0.00001; I2= 77%; 47,533 participants) (Figure 7)23, 26, 28, 32. A significantly increased PVD risk was identified among the SSc cohort (HR, 5.23; 95% CI, 4.25 to 6.45; p<0.00001; I2?=?0%; 26,040 participants) (Figure 8)18, 26, 30.
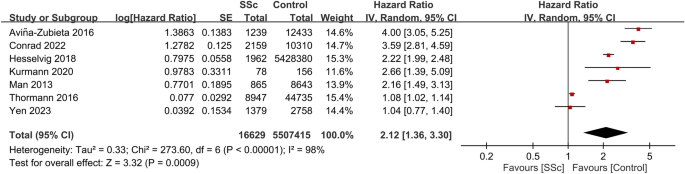
Forest plot showing the association between systemic sclerosis (SSc) and cardiovascular disease (CVD) risk. CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
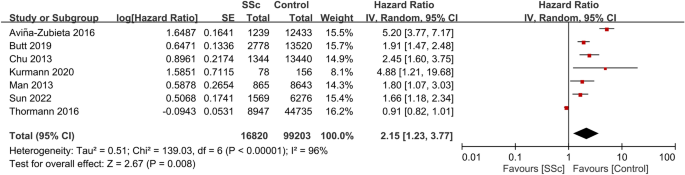
Forest plot showing the association between systemic sclerosis (SSc) and risk of myocardial infarction (MI). CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
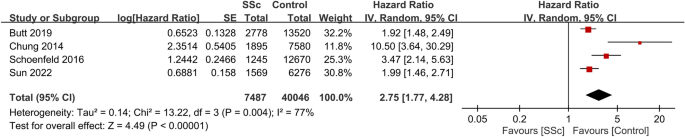
Forest plot showing the association between systemic sclerosis (SSc) and the risk of venous thromboembolism (VTE). CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
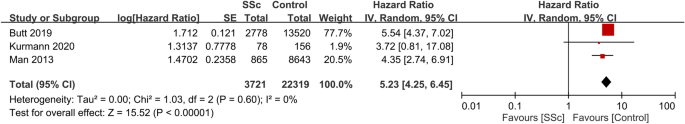
Forest plot showing the association between systemic sclerosis (SSc) and peripheral vascular disease (PVD) risk. CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
Regarding other heart-related events (Figure 9)23, 26, 30heart failure was more common among SSc patients, HR 2.68 (95% CI: 2.28 to 3.15, p≤0.00001, I)2= 14%, 24,377 participants). The occurrence of atrial fibrillation (AF) was also higher in the SSc group (HR: 1.62 95% CI: 1.4-1.89, p << 0.00001, I)2±0%, 24,143 participants). The risk of pacemaker implantation was increased among SSc patients when compared to controls (HR: 1.83 95% CI: 1.32 to 2.53, p = 0.0003, I)2= 6%, 24,143 participants).
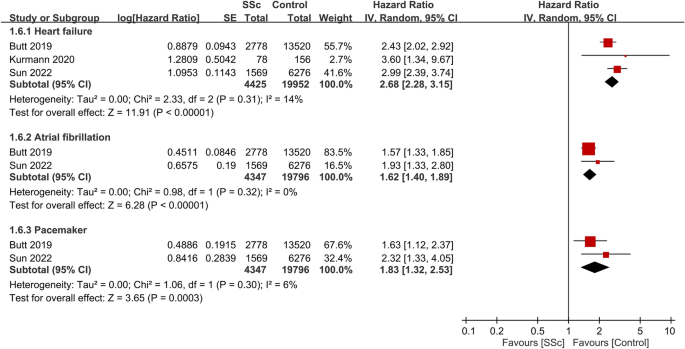
Forest plot showing the association between systemic sclerosis (SSc) and the risk of other heart-related complications. CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
Sensitivity analysis
Sensitivity analyzes aimed at ensuring the robustness of the results confirmed the consistency of all results. Even if one study was omitted from the analysis, the overall results did not change significantly. This consistency emphasizes the reliability of our conclusions and the absence of undue influence from individual studies.
Funnel plot results
For stroke risk, evaluation of the funnel plot showed an asymmetrical distribution of included studies, suggesting the presence of significant publication bias (Figure 10). Funnel plots were not evaluated for other outcomes as there were fewer than 10 studies.
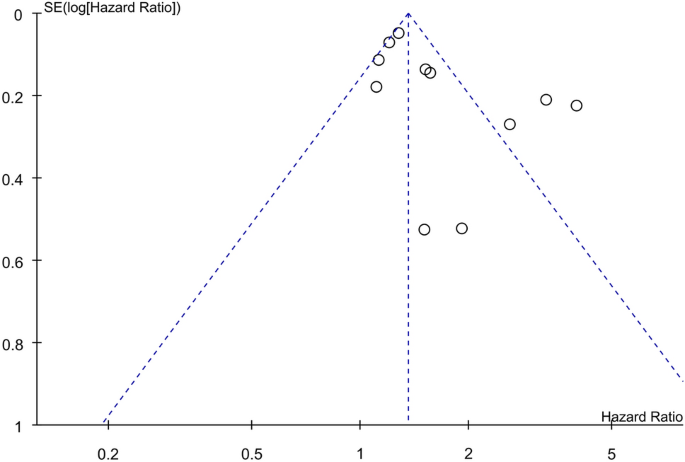
Funnel plot showing potential publication bias for the association between systemic sclerosis (SSc) and stroke risk. CI Confidence interval, Ⅳ inverse variance, S.E. Standard error.
[ad_2]
Source link






