
[ad_1]
My colleagues and I have designed a wireless, ultra-thin pacemaker that uses light to act like a solar panel. This design not only eliminates the need for batteries, but also minimizes disruption to the heart’s natural function by molding to the heart’s contours.
Our research was recently published in a journal Natureoffers a new approach to treatments that require electrical stimulation, such as cardiac pacing.
A pacemaker is a medical device implanted in the body to regulate heart rhythm. These consist of an electronic circuit with a battery and leads that are fixed to the heart muscle to stimulate the heart muscle.
However, the lead can break and cause tissue damage. The position of the lead cannot be changed once implanted, which limits access to other areas of the heart. Pacemakers use hard metal electrodes that can also damage tissue when restarting the heart or regulating arrhythmias after surgery.
Our team envisioned a leadless, more flexible pacemaker that could precisely stimulate multiple regions of the heart. So we designed a device that converts light into bioelectricity, or electrical signals generated by heart cells.
Thinner than a human hair, the pacemaker is made of optical fibers and silicone membranes that Tian’s lab and colleagues at the University of Chicago’s Pritzker School of Molecular Engineering spent years developing.
Frame border=”0″allowfullscreen=”allowfullscreen”>
Unlike traditional solar cells, which are typically designed to harvest as much energy as possible, the device can be fine-tuned to generate electricity only where light hits it, allowing precise control over heartbeats. did. This was achieved by using a layer of very small pores that can trap light and electrical current. Only the heart muscle exposed to the light-activated pores is stimulated.
Our device is so small and light that it can be implanted without opening the chest.
We successfully implanted it into the hearts of rodents and adult pigs, adjusting the beats of different cardiac muscles. Since the pig heart is anatomically similar to the human heart, this result indicates the potential for our device to be applied to humans.
why is it important
Heart disease is the leading cause of death worldwide. Each year, more than 2 million people undergo open-heart surgery to treat heart problems, including the implantation of devices to regulate heart rhythm and prevent heart attacks.
Our ultra-lightweight device gently conforms to the surface of the heart, allowing for minimally invasive stimulation and improved pacing and synchronized contractions. To reduce postoperative trauma and recovery time, our devices can be implanted using minimally invasive techniques.
What is not known yet
Currently, our technology is best used first for cardiac emergencies, such as post-surgical cardiac restart, heart attack, and ventricular defibrillation. We continue to study its long-term effects and durability in the human body.
The internal environment of the body is rich in fluids, which are hindered by the constant mechanical movement of the heart. This can impair the functionality of your device over time.
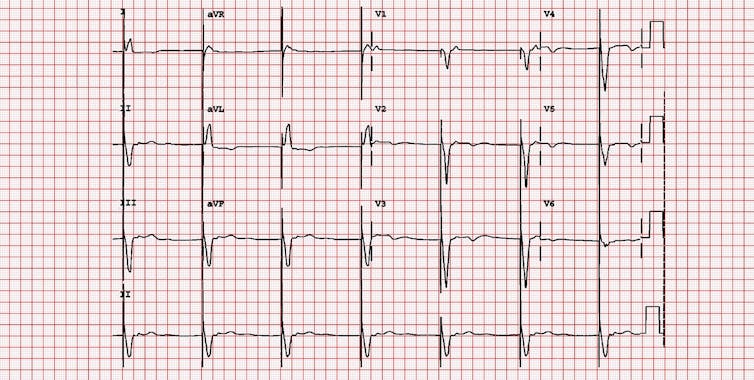
Michael Rosengarten BEng, MD.McGill/EKG World Encyclopedia
Additionally, researchers do not fully understand how the body responds to long-term exposure to medical devices. Scar tissue that forms around the device after implantation can reduce the sensitivity of the device. We develop special surface treatments and biomaterial coatings to reduce the possibility of rejection.
When our device fails, it produces a non-toxic substance called silicic acid that the body can safely absorb, but to ensure safety and effectiveness, we need to know how the body reacts to long-term implantation. It is essential to assess how you will react.
what’s next
We are improving the natural rate of dissolution in the body to enable long-term implantation and tailor the device to each patient. We are considering enhancements to make the device compatible as a wearable pacemaker. This involves incorporating wireless light-emitting diodes (LEDs) under the skin that are connected to the device via fiber optics.
Our ultimate goal is to expand the scope of what we call photoelectroceuticals beyond cardiac care. This includes neurostimulation, neuroprosthetics, and pain management to treat neurodegenerative conditions such as Parkinson’s disease.
Research Briefs are short summaries of interesting academic research.![]()
Pengju Li, Ph.D. Candidate in Molecular Engineering, Pritzker School of Molecular Engineering, University of Chicago
This article is republished from The Conversation under a Creative Commons license. Read the original article.
[ad_2]
Source link






