[ad_1]
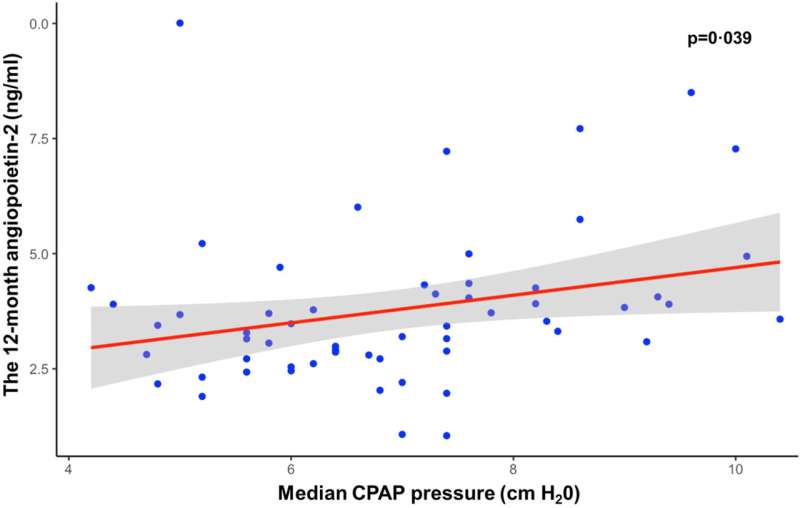
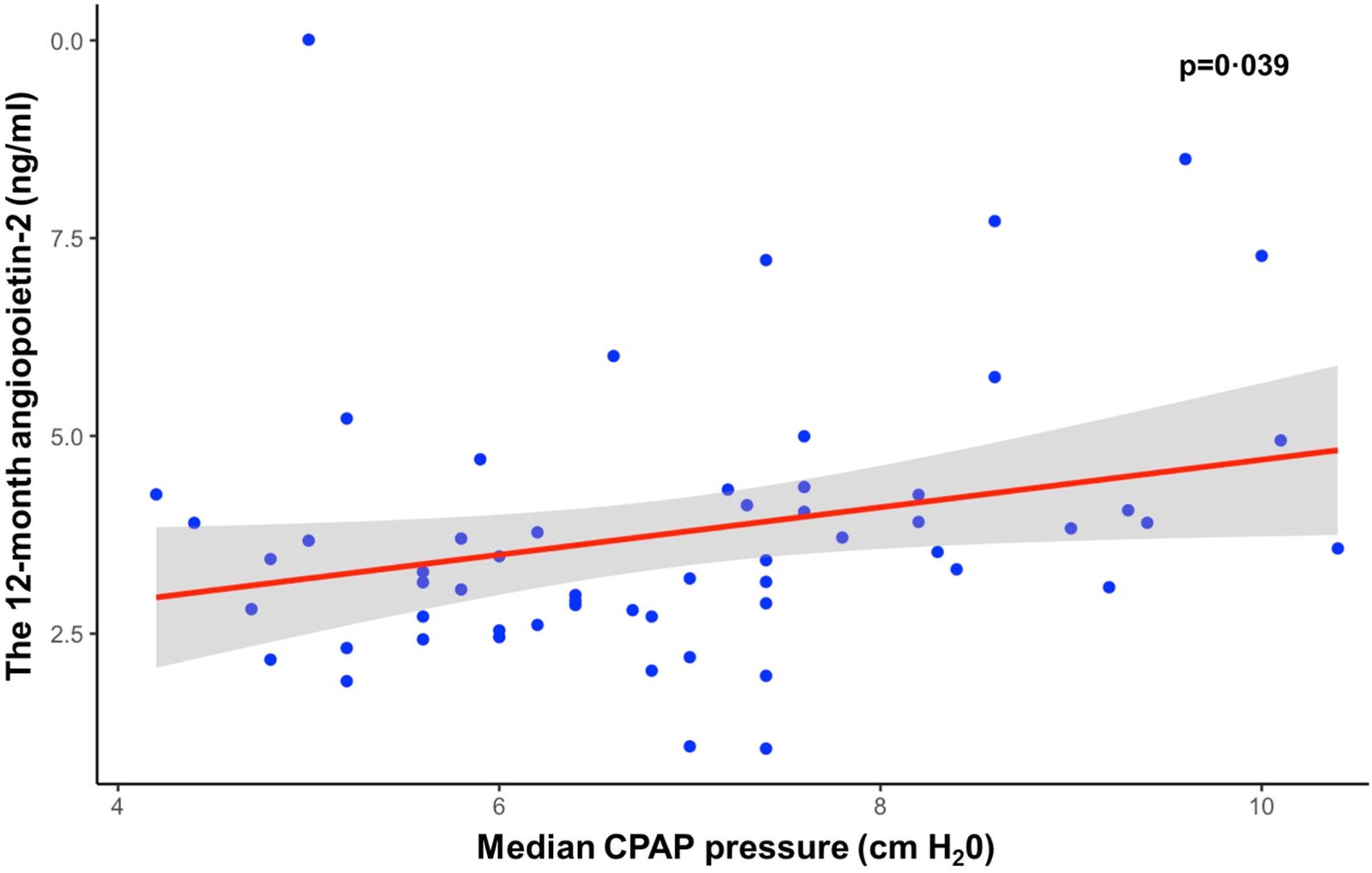
Circulating levels of angiopoietin-2 are associated with median CPAP pressure in obstructive sleep apnea patients after coronary revascularization (linear regression slope 0.30, 95% CI 0.03, 0.57, p = 0.039 ). The shaded area represents the 95% confidence band. CPAP, continuous positive airway pressure. credit: e-biomedicine (2024). DOI: 10.1016/j.ebiom.2024.105015
A study of people with obstructive sleep apnea found that high CPAP pressures may explain why machines fail to lower the risk of heart disease, which is about two to three times higher than average. Suggested.
“While CPAP machines are highly effective in treating obstructive sleep apnea and are great for improving sleep and reducing daytime fatigue, they have not shown the reduction in heart disease that we had hoped for. We still don’t know why,” says Sanja Jelic. Doctor. A critical care medicine specialist and sleep researcher at Columbia University Vagelos College of Physicians and Surgeons.
CPAP and inflammation
Obstructive sleep apnea, which affects approximately 25% of adults in Western society, occurs when the muscles of the upper airway relax and the airway collapses during sleep. The subsequent infiltration of oxygen often wakes people up, and in extreme cases it wakes up every two minutes, leading to daytime fatigue.
“This can go on forever, with oxygen levels rising and falling throughout the night,” Jerick says. Repeated drops in oxygen levels lead to increased inflammation, which is thought to cause an increased risk of heart disease associated with obstructive sleep apnea.
Because CPAP machines restore normal breathing during sleep (by using positive air pressure to keep the upper airways open), researchers believed that CPAP also reduced patients’ risk of heart disease. .
But a few years ago, research conducted by Gerrick and Dr. Daniel Gottlieb, a collaborator at Brigham and Women’s Hospital, began to suggest problems with this hypothesis. A study designed to understand the effects of CPAP on the body found that CPAP use did not reduce levels of the pro-inflammatory factor angiopoietin-2. Previous studies have linked high levels of Ang2 to increased rates of stroke, coronary artery disease, vascular disease, and mortality.
“This was a surprise. We naturally expected that once the intermittent hypoxia was resolved with CPAP, the Ang2 release would stop, but it actually got worse,” says Jelic.
Around the same time, results from three randomized trials of CPAP came in, none of which found any cardiovascular benefits for the machine.
Jerick said the pattern of Ang2 and other biomarkers in CPAP users is similar to that of patients on hyperbaric ventilators, and that CPAP pressure may be the reason the expected reduction in heart disease did not materialize. We hypothesized that this could be explained by the height of .
new analysis
To dig deeper, Geric and Gottlieb took a closer look at participants in the first trial, RICCADSA, conducted in Sweden with 189 people with obstructive sleep apnea. The researchers analyzed the stored blood samples for Ang2 and other inflammatory markers and compared those numbers to CPAP adherence, median CPAP pressure, and the patients’ heart health after one year.
Their analysis showed that Ang2 levels remained elevated in CPAP users, confirming Gerrick’s previous findings in a small study, and also found that high Ang2 levels were It was found that the risk of cardiovascular disease increases after a month.
The researchers then discovered that patients with the highest Ang2 levels were those using higher CPAP pressures.
Standard CPAP prescriptions use pressures ranging from 4 to 20 cm H.2The median pressure of O varies within that range. In this study, participants with a median CPAP pressure of 4 to 7 had fewer cardiovascular events compared to participants who used pressures of 8 or higher. No correlation was found between Ang2 levels and the number of hours he used CPAP during the night.
“This suggests that there is something in the lungs that responds to CPAP pressure that perpetuates rather than reduces the inflammation associated with obstructive sleep apnea,” says Gerrick.
Effect of pressure
Because CPAP is known to expand the lungs, although not as dramatically as a ventilator, Jerick believes that the expanded endothelial cells in the lungs release extra Ang2. Although it is not possible to directly measure Ang2 release from human lungs, stretching other tissues in clinical tests rapidly increases Ang2 release from endothelial cells.
Jerick is already changing the way he uses CPAP for his sleep apnea patients.
“I’ve been prescribing lower pressures,” she says. “We’re making careful adjustments to see which pressures eliminate most of the blocking events, and it’s working just fine.”
Most doctors now adjust CPAP pressure to eliminate all obstructive episodes during sleep. But even if some obstructive symptoms occur, Jerrick says, lowering the pressure may reduce Ang2 and provide the same sleep and fatigue improvements.
“That’s something that needs to be tested in a randomized trial,” she says.
For more information:
Yuksel Peker et al., CPAP may promote an endothelial inflammatory environment in sleep apnea after coronary revascularization, e-biomedicine (2024). DOI: 10.1016/j.ebiom.2024.105015
Provided by Columbia University Irving Medical Center
Quote: Why doesn’t CPAP reduce heart disease? (February 26, 2024) From https://medicalxpress.com/news/2024-02-doesnt-cpap-heart-disease.html February 26, 2024 get to date
This document is subject to copyright. No part may be reproduced without written permission, except in fair dealing for personal study or research purposes. Content is provided for informational purposes only.
[ad_2]
Source link






