[ad_1]
The move could pave the way for thousands of new prescriptions and result in billions of dollars in increased spending, analysts said.
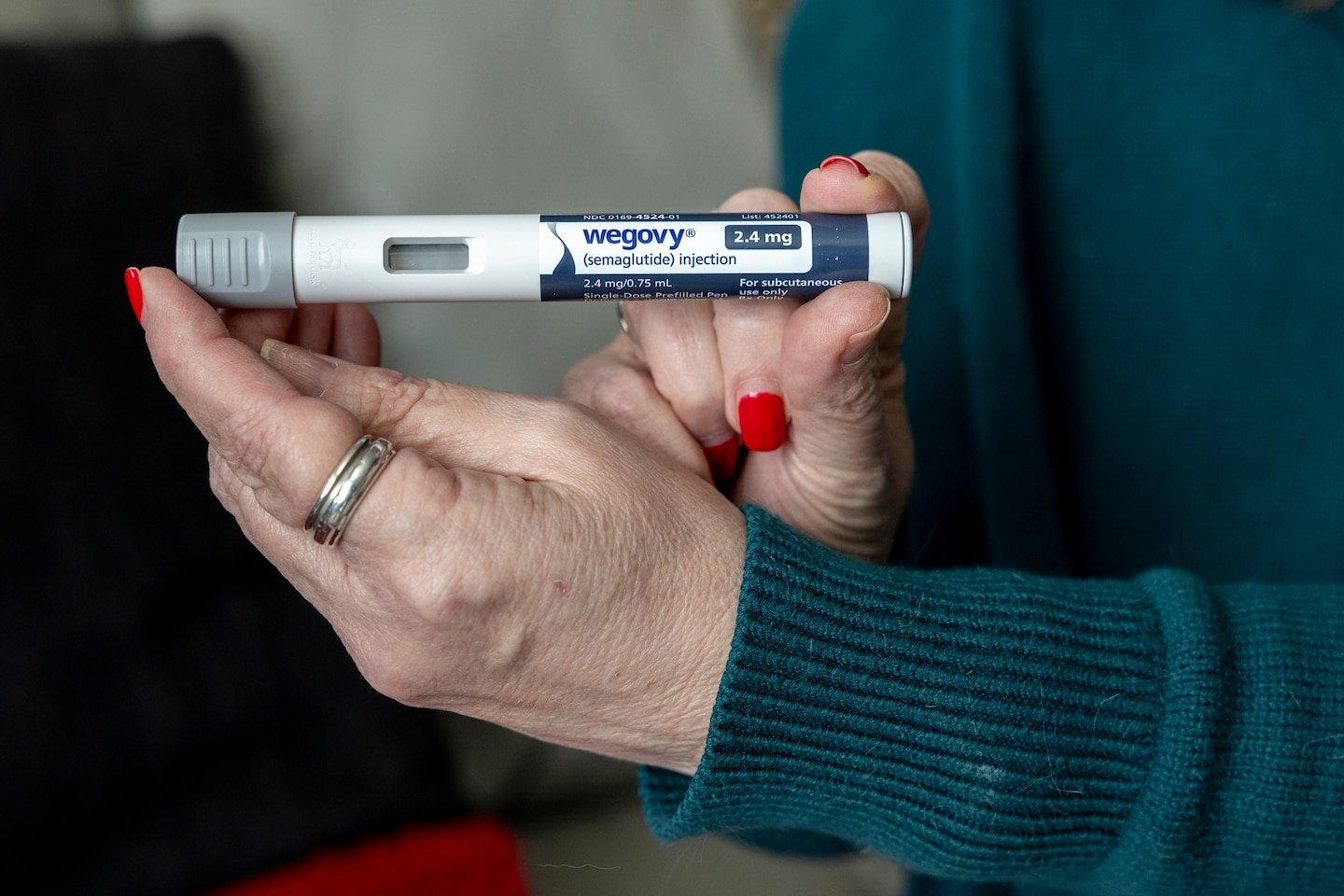
In fact, the guidance opens the door to broader coverage of Novo Nordisk’s brand name for its obesity drug semaglutide, Wegoby. The U.S. Food and Drug Administration this month approved label changes that will allow Wegovy to be used to reduce the risk of cardiovascular events in people who are overweight or obese and have heart disease.
A recent study showed that Wegovy reduced the risk of heart attacks, strokes, and other problems by 20% in such patients compared to a placebo or dummy drug. Cardiologists and other experts said using semaglutide to reduce the risk of the often fatal or disabling condition could change the way heart patients are treated.
Wegovy costs over $1,300 per month or $16,000 per year.
Part D plans could begin covering the drug “as soon as this year,” said Tricia Newman, a Medicare policy expert at KFF, a nonprofit organization that studies health policy.
“Medicare plans may be reluctant to act quickly to cover Wegobee given the relatively high prices, especially since premiums cannot be adjusted until next year,” she said. Ta.
Even if a plan allows coverage, those who meet the criteria may still face other limitations. Plans could require higher copays, prior authorization or step therapy, which requires patients to try lower-cost drugs before moving on to new treatments, Newman said.
Medicare Part D plans are prohibited by law from covering obesity drugs used solely for chronic weight management, and that will not change, CMS officials said.
A spokesperson for American Health Insurance Plans (AHIP), an industry group, said private insurers are evaluating the guidance and the new indication for Wegoby before making coverage decisions.
Pharmaceutical companies and obesity advocacy groups are pushing for expanded coverage, including legislation that would require Medicare to pay for obesity drugs.
The question is whether the high drug costs will be offset by savings from lower medical costs associated with obesity and now heart disease.
One remaining obstacle to widespread use is the drug’s limited supply, which has been in short supply for more than a year, according to the FDA. Novo He said Nordisk officials are working to increase production and access.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Education Media Group. AP is solely responsible for all content.
[ad_2]
Source link






